CMS is investigating Temple University Hospital following the death of a homeless patient due to concerns about the quality of care provided.
In a troubling case that has garnered the attention of state and federal authorities, Temple University Hospital’s handling of a high-risk patient has raised significant concerns about patient safety and medical ethics. An investigation was prompted after a patient, who had no home to return to, was discharged and subsequently suffered severe consequences due to the hospital’s neglect.
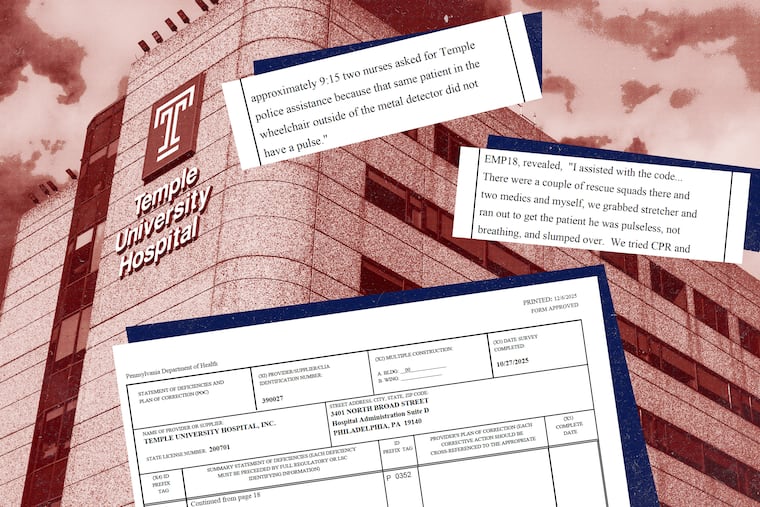
On October 3, the patient was discharged and wheeled to a bench outside the hospital, despite his known high risk of falling. Hospital staff left him alone, where he remained for an extended period before ultimately falling to the ground. A security officer later discovered the man lying unresponsive on the pavement, and though he was returned to the emergency department, he was once again left unattended in a wheelchair. Tragically, he was later found slumped over, unresponsive, and without a pulse, ultimately passing away five days later.
According to a report from the Pennsylvania Department of Health, the incident is reflective of serious violations of the Emergency Medical Treatment and Labor Act (EMTALA), which mandates that all patients seeking emergency care must be medically evaluated and stabilized before discharge. The department’s findings indicated that hospital staff engaged in a practice commonly referred to as “patient dumping,” wherein vulnerable patients are inadequately treated and released without appropriate care.
The Centers for Medicare and Medicaid Services (CMS) has confirmed that it is also investigating the incident, adding to the scrutiny Temple University Hospital is currently facing. The violations could result in severe penalties, including the risk of hefty fines or the potential loss of the facility’s Medicare license.
Temple University Hospital has acknowledged the failure to adhere to established protocols, asserting that the patient should not have been released without proper medical clearance. Staff members indicated that the patient’s condition had not been adequately assessed, and protocols dictating patient mobility evaluations for high-risk individuals were not followed.
Experts in healthcare law have provided insight into the broader implications of this incident, emphasizing that it is not merely the fault of individual staff members, but rather indicative of systemic issues, such as understaffing and operational bias against marginalized patients. The hospital’s environment and culture play crucial roles in patient care, underlining the need for leadership to prioritize safety and adequate staffing.
While some reforms have been promised by the hospital, the incident highlights the ongoing challenges that hospitals face in delivering equitable care, especially to populations experiencing homelessness. As Temple University Hospital treats a vulnerable patient demographic, these systemic problems underscore a pressing need for transformative practices in healthcare to prevent recurrence of such tragedies.